Coronis Health, FQHC & CHC
FQHC & CHC Billing
Coronis Health understands the unique nuances of billing and coding for Federally Qualified Health Centers (FQHCs) and Community Health Centers (CHCs).
Our experienced FQHC medical billing team remains constantly vigilant and compliant amid the changing chorus of governmental/carrier billing and documentation regulations, as well as compliance requirements for Medicare and Medicaid.
Want to know how to use financial reports and analytics to drive operational change within your FQHC? Check out our webinar.
Specialized Solutions, Global Capabilities
Risk-Free Financial Checkup
We Find Missing Revenue In 95% Of Our Reviews
– Comprehensive review of your complete revenue cycle
– Compare key metrics against competitors in your specialty
– Review patient and insurance A/R, charges, and fee schedules
*Rate is based on collections volume
Case Studies
FQHC & CHC Billing
Specializing In
Testimonials
-
36+
Years of Industry Experience
-
100+
Hospital Partners
-
1B
Claims Processed per Year
-
$20000000000
In Charges
-
$4700000000
In Payments
Size Matters! More is Always More!
Services

What Makes Us Different
Coronis Health is a global company with a personal, high-touch service. We brought the most innovative and thought-advancing leaders in hospital and facility medical billing and revenue cycle management together to progress this industry into the modern, technological age. Because of our agility and scalability, we can work with a hospital or facility of any size.
-
Best of the best in medical billing, joining forces
Coronis Health is comprised of the top medical billers in the country pooling their global resources to bring customers the best in medical billing and revenue cycle management. With over 100 years of combined experience in various niches including hospitals of all sizes, Coronis offers customers tailored solutions and high-touch relationships you won’t find at a “Big Box” medical billing company.
-
Technological innovators
Coronis Health was recognized as one of the top 10 medical billing & coding solutions providers (source). We are fully integrated with the latest software so we input coding instantly, and execute collections fast and efficiently. We can go from contract to onboarding your systems in a matter of weeks, not months. Our team works quickly to get medical billing and A/R follow-up running so you can start collecting and hitting and beating financial targets. We’ve developed an advanced technological system that learns how to collect, who to collect from, and how to get that “last $” in an efficient and cost-effective manner.
We work with the latest software and any system you use. We input coding instantly and execute collections fast and efficiently. Our Artificial Intelligence-based software means constantly finding new ways to discover lost revenue and improve your collections.
-
Focused on your independence
We make sure you are 100% compliant and able to receive patients and bill either out-of or in-network. Coronis Health goes after the last dollar using our seasoned team of tireless and tough negotiators. You’ll receive timely, relevant, and accurate information in a way you can understand. We don’t help you just get money, we help you financially grow.
-
Personalized touch
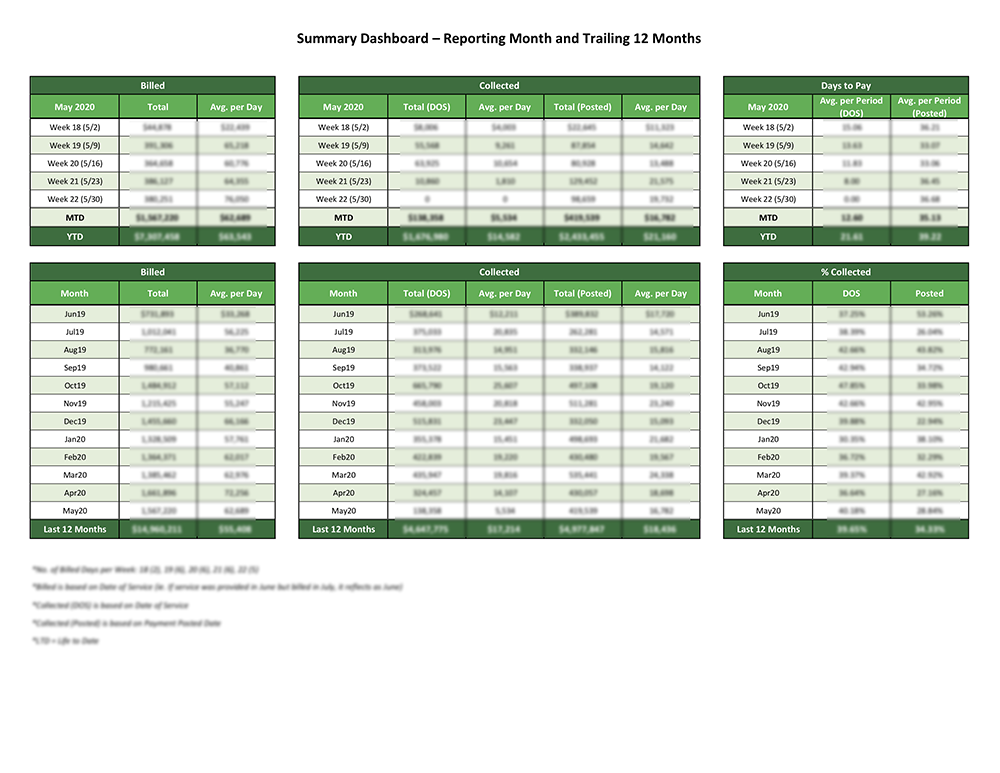
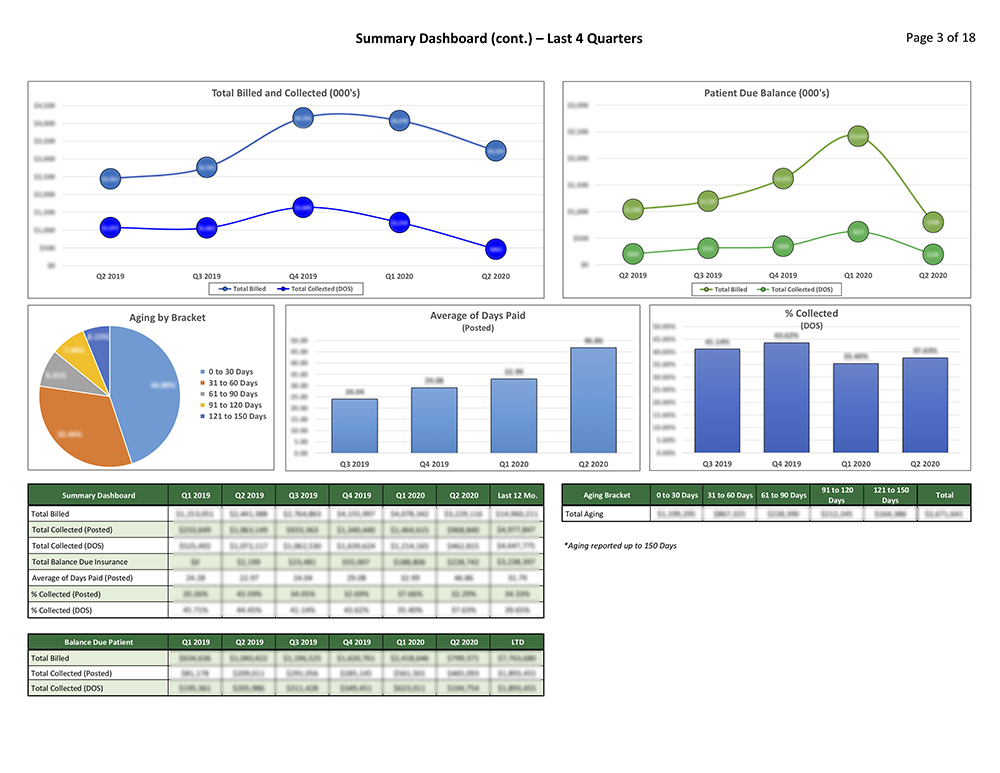
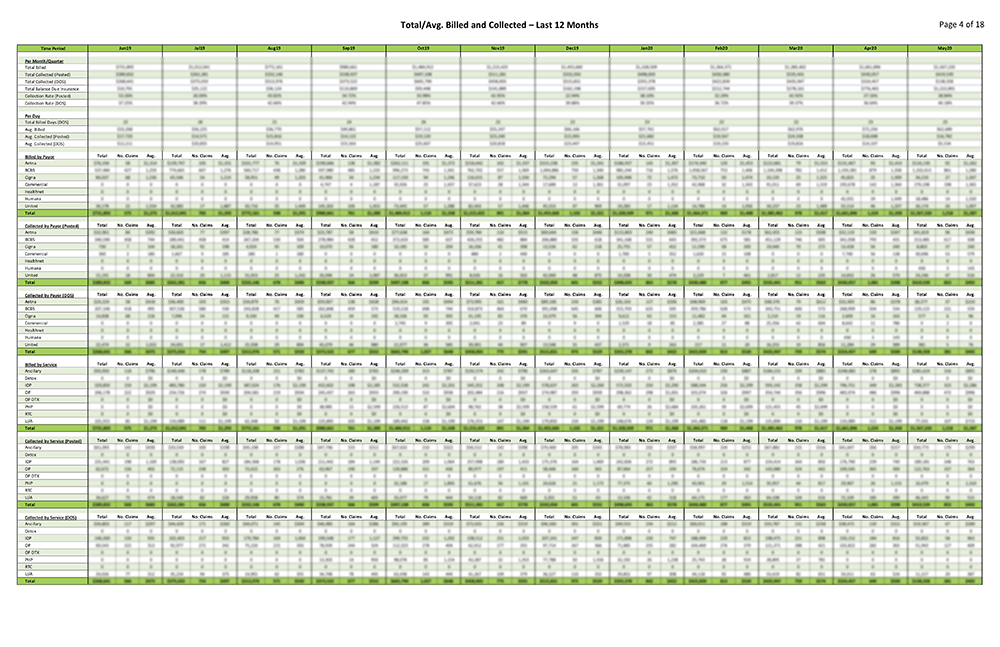
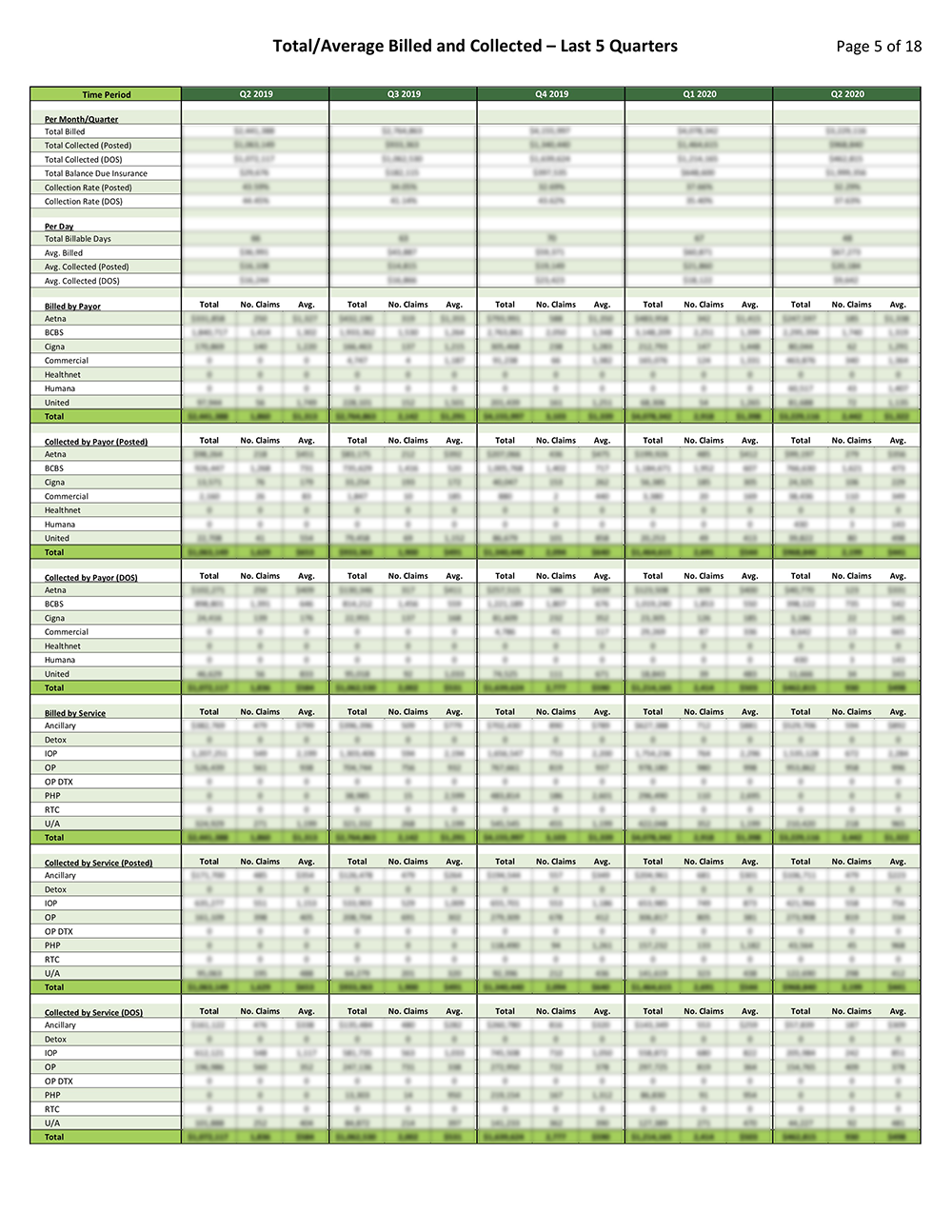
With Coronis Health on your side, you’re paired with an experienced US-based account manager who understands how to help your facility succeed. You aren’t just a number, you’re on a first-name basis and a phone call away. Our transparency guarantee ensures that you see what we see. We deliver reports that are clear and digestible and allow you to make the best decisions for your practice.
More About Coronis Health
FQHCs and CHCs know that their most important financial asset is their billed services and accounts receivable. This asset needs to be safeguarded, well-organized, tightly managed, and carefully maintained by a professional team possessing a perfectionist approach to execution, accuracy, follow-up, and timeliness. And of critical importance, center administrators need to remain constantly vigilant and compliant amid the changing chorus of governmental/ carrier billing and documentation regulations and compliance requirements including Medicare and Medicaid.